It’s Saturday night and you’re perusing Instagram. Nothing special, just looking at some memes or a funny video of a cute pup. All of a sudden, you find a post about a “birth control cleanse.” This freaks you out because, as someone who hopes to have children in the future, you have never heard of this before. You start frantically googling “birth control cleanse” and “birth control detox” and pages upon pages come up about Premama Wellness and how to reset your hormones after getting off the pill. You feel panicked. Your doctor didn’t tell you about this!
Before we go any further, take a deep breath and let’s look at the different types of birth control and how they work. There are actually 18 different forms of birth control (Figure 1). While some of these methods are clear-cut (like abstaining from sex, getting your tubes tied, and condoms), other types are less well-understood. Many people understand that some of the methods like the implant, the pill, and the IUD release hormones into their body and this – somehow – prevents pregnancy. Unfortunately, there is a lot of confusion about how these hormones affect the natural female reproductive cycle. Let’s delve into the natural female menstrual cycle first.
Image created by Eliza Thulson.
The Menstrual Cycle
The menstrual cycle is just that – a cycle. The first day of the cycle starts when bleeding begins and ends when the next period begins. This whole cycle is typically 28 days long, but the period is only part of it. The cycle is broken up into two phases – the follicular phase and the luteal phase (Figure 2).
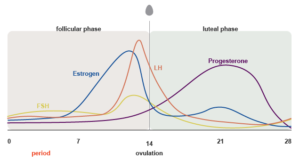
Image created by Eliza Thulson.
During the follicular phase, the hypothalamus (a small part of the brain responsible for maintaining bodily functions such as temperature, thirst, and hunger) sends a message to the pituitary gland (a small organ near the hypothalamus that produces and releases hormones). The message from the hypothalamus tells the pituitary gland to release a hormone called follicle stimulating hormone, or FSH. FSH travels through the body to the ovaries and prompts the ovaries to produce 5-20 follicles, which are tiny nodules on the surface of the ovary that each house an immature egg. The growth of these follicles stimulates the lining of the uterus to thicken in preparation for a potential pregnancy and causes a rise in the hormone estrogen. When estrogen levels reach a certain, sustained amount, the hypothalamus releases another hormone called gonadotropin-releasing hormone (GnRH). GnRH triggers the pituitary gland to release even more FSH and produce another hormone, luteinizing hormone (LH). As levels of LH surge, ovulation occurs (around day 14) and an egg is released from the ovary into a fallopian tube, toward the uterus (Figure 2). Unless the egg is met by sperm in the uterus, it will die.
Remember that the egg was housed in a follicle on the ovary? When ovulation occurs, the egg bursts from the follicle and leaves the ruptured follicle behind on the ovary’s surface. This event marks the start of the luteal phase. This ruptured follicle turns into a structure called the corpus luteum, which produces a lot of a hormone called progesterone and a small amount of estrogen. The high progesterone levels and lower amounts of estrogen cause the pituitary gland to stop releasing FSH and LH. At this point, either one of two steps can occur:
- If the released egg is not fertilized, the corpus luteum eventually dies around day 22 of the cycle, and thus progesterone and estrogen are no longer produced. The lack of these hormones causes the lining of the uterus to fall away, which is recognized as bleeding, or menstruation. The cycle then begins again (Figure 2).
- If the released egg is fertilized, it begins producing human chorionic gonadotropin (HCG), the hormone recognized in urine by pregnancy tests. HCG mimics LH by acting on the corpus luteum to keep producing progesterone, which prevents the release of FSH and LH, and thus inhibits menstruation.
Hormonal Birth Control
So, how does hormonal birth control affect the menstrual cycle? The answer is that it depends on the birth control method used, but most are pretty similar. Hormonal birth controls contain either estrogen and progestin (a synthetic form of progesterone) or just progestin. The pill, shot, patch, implant, IUD, and ring work by releasing consistent levels of these hormones, which can be absorbed through your body (Figure 3). The consistent levels of estrogen and/or progestin prevent FSH and LH from being released from the pituitary gland, resulting in failure of follicles to mature, and thus preventing ovulation. Without the release of an egg from the ovary, fertilization cannot occur. This process essentially mimics pregnancy, when FSH and LH are not produced and the body does not menstruate. The consistent levels of hormones also thicken the cervical mucus, creating a barrier to sperm.
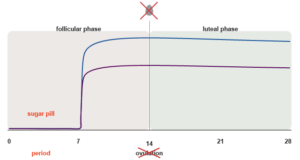
The really interesting (and convenient) thing about birth control is that it can be used to prevent bleeding not just for three weeks, but for much longer. For example, hormonal IUDs such as Kyleena and Mirena can work for 5-7 years and release consistent levels of estrogen and progestin for this entire time. The constant levels of estrogen and progestin prevent menstruation, sometimes for 3 weeks or sometimes longer. The pill is usually taken for 3 weeks and then stopped for one week. During this one week, the levels of estrogen and progestin drop sharply, inducing menstruation. However, this one week of bleeding can be skipped by simply continuing to take the pill. Likewise, the vaginal ring can simply be replaced every 3-5 weeks without taking a break in between replacements.
Benefits of Hormonal Birth Control
I bet you’re wondering – but is this safe? Isn’t getting a period normal and healthy? Yes, and – yes. While it’s true that women’s bodies naturally go through the menstrual cycle, unless you are trying to get pregnant or have other underlying medical issues, skipping your period is perfectly fine. Multiple studies have found that there are no health or safety differences between women who continuously take birth control vs those who cycle. In fact, women who do not cycle have reported fewer menstrual-related symptoms, such as cramps, migraines, and moodiness. There are other benefits to taking birth control continuously as well – taking hormonal birth control lowers the risk of developing endometrial and ovarian cancer and can treat symptoms of other syndromes such as polycystic ovary syndrome and endometriosis.
You’re thinking this is all great – but what about all the terrible things people say happen after getting off birth control – like acne, moodiness, and heavy periods? Is fertility affected by the synthetic hormones? Studies have found that fertility is not affected by continuous birth control use and that the ability to get pregnant is also unaffected. While it can take 1-3 months for a period to make its appearance, most women ovulate 2 weeks after stopping birth control. The hormones from birth control do not stay in the body, but it can take a few weeks for the body to return to its regular cycle. Luckily, there are many women who do not experience any side effects from discontinuing hormonal birth control, and are able to conceive soon after.
What is a “Birth Control Cleanse?”
If you are ready to have a baby, or you want to quit birth control for personal reasons you may have come across those Instagram posts about birth control cleanses/detoxes. You do not really know what it is, but you wonder if you need this – especially since it seems like so many Instagram influencers highly recommend it! Let me beat you to the punch line: although it sounds great, there is not a magic drink or pill that can re-balance your hormones after stopping birth control.
A birth control cleanse is typically some type of drink mix promoted as an aid to reset your body following discontinuation of hormonal birth control. Companies like Premama Wellness sell this $59.99 product containing 28 powder packets, which are supposed to both “prep the body for pregnancy by balancing hormones and stimulating uterine health” as well as “nourish, support, tone, and gently cleanse the liver and uterus.” (You really do not need to tone or cleanse your uterus, let alone your liver, which is quite literally the detoxification system of the body.) The mix basically contains the same things as prenatal vitamins – vitamin C, vitamin E, and folic acid – but their added ingredient, chasteberry (Figure 4), is what they say really does the trick. After some digging around on their website, a blog post finally reveals their claim to fame with chasteberry: a natural source of progesterone that will balance your hormones and help your period become normal again in preparation for pregnancy. While there is some evidence that chasteberry can have indirect effects on various hormones such as estrogen, progesterone, and prolactin, and can also help relieve premenstrual syndrome (PMS) symptoms, there is little evidence to support its role in promoting fertility. Studies concluding that chasteberry can promote fertility have been notably small and focus mostly on luteal phase disorders, include other herbal supplements whose effects on fertility and pregnancy are unclear, and have yet to go to clinical trials to determine a dosage.

Unfortunately, companies such as Premama Wellness take advantage of those who struggle with infertility and desire to conceive by spreading misinformation. The evidence that these companies cite for chasteberry in promoting fertility is weak, inconclusive, and has yet to go to clinical trials. For those who do not wish to conceive, these companies are using scare tactics to make them think that something is wrong with them. Many of these products are supported by NMDs, or doctors of naturopathic medicine, and social media “influencers.” While NMD may sound similar to a medical degree (MD), there are major differences in the requirements for entrance exams, residencies, and lecture and study hours. Currently, each state in the US has different laws about what an NMD can do – in some states, NMDs can prescribe medications, perform minor surgeries, and draw blood, but in others, are restricted to only providing nutritional advice or homeopathy. The lack of nationwide regulations for NMDs is both concerning and problematic.
The bottom line is this: if you think you have some type of hormonal issue, go see your doctor (an MD). Because birth control affects everyone differently, what has worked for someone else might not work for you. Refrain from getting your medical advice from the internet, an Instagram influencer, or anyone else. Save yourself time, money, and emotional stress by speaking with your healthcare provider first.
Peer edited by Rita Meganck and Marguerite Little