While COVID-19 is the latest pandemic to affect humanity, it certainly isn’t the first. From smallpox in the 1600s, to the Spanish flu of 1918, the United States has repeatedly been hit by deadly diseases. Over time, epidemiologists have created mathematical models using information from previous pandemics in order to predict characteristics of on-going diseases. These models have proved to be an important component in the fight against pandemic spread, driving government policies and helping to minimize the strain on our healthcare system.
Why model pandemics?
Why spend all this time trying to predict the course of a pandemic? These models are essential in telling us how certain measures, like social distancing or banning large gatherings, can help reduce spread and death rate. Models can also help determine when and for how long these measures should be carried out. Information from models is crucial in reducing the amount of infections, deaths, as well as strain on hospitals. Furthermore, they help us in determining how to allocate limited resources, such as hospital beds and ventilators, which have been in short supply, by modeling the course of a pandemic in different regions.
Types and characteristics of pandemic models
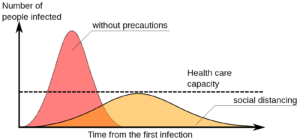
Epidemiologists and mathematicians select from a variety of different pandemic models based on the characteristics of the disease and the particular population of interest. The most basic pandemic model is called the S-I-R model, which refers to the number of susceptible individuals, number of people who are infectious, and people who have recovered (or have been removed due to death) from the disease and are no longer infectious. Using these three characteristics, this model provides a relatively simplistic way of computing the number of people who will become infected with the disease over time. Importantly, this model demonstrates just how influential limiting social contact is to hampering disease spread. If an infected person self-isolates, they aren’t capable of spreading the disease, and in terms of disease modeling they have essentially skipped ahead to the “recovered” group. Social distancing therefore greatly contributes to the “flattening of the curve” of hospitalizations, making it easier for hospitals to deal with the influx of patients.
While there are other variations on this model, such as those that assume a person doesn’t receive immunity upon recovering from the disease (S-I-S), or where immunity only lasts for a short period (S-I-R-S), all of these models calculate a variable known as R0 (pronounced “R-nought”). R0 represents the basic reproduction number of a disease, and tells us exactly how contagious a particular disease is. With an R0 of 1, one person will spread the disease to exactly one other person, making it unlikely for a widespread outbreak. When R0 is greater than 1, however, the disease has potential to spread exponentially; for example, an R0 of 2 means one person will spread to two others. Certain diseases like measles are highly contagious (R0 of around 12-18), while the season flu is less so (R0 of around 1.3). Preliminary studies for the R0 of COVID-19 vary greatly depending on the location and time since disease onset, but is likely somewhere around 2.5, making it somewhere in the middle as far as its level of contagiousness.
Current models of COVID-19 in the United States
While there are many S-I-R models available for the COVID-19 pandemic in the United States (for example, here and here), the Institute for Health Metrics and Evaluation (IHME) at the University of Washington took a slightly different approach, and has been modeling COVID-19 projections using reported death rates instead. This model circumvents limitations in S-I-R models that fail to consider effects of government-mandated actions, as well as lack of COVID-19 testing. According to IHME, US deaths could reach 81,000 by July, while the most dire model from the CDC (in which it was assumed no measures were taken to slow the spread of the disease) predicted death tolls up to 1.7 million.
The future of COVID-19
Pandemic modeling is far from an exact science, due to the fluid nature of diseases as well as on-going measures taken by governments to prevent disease spread. It’s important to keep in mind, however, that models often represent a “worst case” scenario that are used to motivate governments into taking action, and shouldn’t necessarily be viewed with skepticism because their predictions turned out to be false. Hopefully, many of the current dire predictions made for COVID-19 will indeed turn out to be overestimations due to preventative measures such as social distancing, travel limitations, and business shutdowns.
Peer edited by Brandon Le