The story behind the story.
This story was inspired by a casual journal club discussion in my lab, centered around a paper with implications on the underlying mechanism of Alzheimer’s disease. During the conversation, my advisor jokingly said, “If I ever can’t tell people from bananas, replace my microglia!” (To be perfectly candid, this comment made sense in the context of discussion.)
This moment stuck with me. I started thinking about how everyone—from my big-hearted, sensitive mother to my 53% cynical advisor—is quietly worried about aging. And of all the possibilities in this inevitable stage of life, neurodegenerative disorders like Alzheimer’s disease seem to expose the most profound fear of all: the loneliness of forgetting.
So, what about people already living with dementia? How should they be cared for in the face of a condition that allows no U-turn? In reading clinical reviews that center these patient’s lived experience, I noticed a consistent theme: acknowledge the disease’s impact, adapt care accordingly, but always prioritize a sense of autonomy. Don’t patronize. Don’t pity. And don’t reduce them to their disease.
That’s what led me to write this story of Dawn Yue. Dawn is the first light of day, the moment the world begins again. Even as parts of her memory fade, she holds onto her core identity: someone who sees clearly, who begins again, and who persists through the fog. Her last name, Yue, means “moon” in Chinese. In contrast to dawn, the moon appears in darkness. It changes phases. It reflects light rather than producing it. More importantly, it reminds us that memory and sense of self—like moonlight—can wax and wane, but still illuminate.
Together, Dawn Yue reflects the experience of dementia itself: a life lived in cycles of clarity and confusion, presence and absence. Just as the sun and moon continue their rhythms whether or not anyone is watching, people with dementia can continue to live full, meaningful lives, even when others see only what’s been lost.

Dawn woke up from – well, is it still called sleep if you feel more tired afterward than before?
It was still dark outside, but the sun would rise in less than an hour. Might as well get up and get ready, she thought. I could use some coffee. She picked out the coffee beans herself—she liked having an equal ratio of uniform and irregularly shaped beans—and placed them in the fancy espresso machine her daughter had given her as an early retirement present. She pressed “double shot” and went to freshen up.
At 6 a.m., her alarm finally rang; the one she’d forgotten to turn off after deciding to rely on her biological clock. The shrill sound gave Dawn a headache that is more intense than usual. She rushed out of the bathroom to silence it, leaving her hairbrush by the dining table in a hurry.
Now dressed for work in her usual crisp, ironed shirt, she looked at herself in the mirror. As she closed the front door behind her, a thought flickered: Something is missing.
The door cracked open again. Dawn stepped back to bring her hairbrush back to the bathroom. It was a beautiful day outside. She was ahead of schedule and decided to treat herself to a cup of coffee from the cart near the hospital.
The door shut once more, leaving behind a lonely espresso machine, beeping for the third time.
First sign: we’ve already talked about this
Dr. Dawn Yue was a professor of Cancer Biology. Today marked the thesis defense of her 20th graduate student, and she was genuinely happy for them.
She walked into the departmental conference room, expecting to find other faculty members from the committee. Instead, two repair technician were adjusting the audio-visual equipment.
Odd. No one had mentioned any scheduled maintenance so close to the start of a defense. Has the defense been moved? Maybe there was an email she’d missed.
Time was running short. She pulled out her phone to check her inbox, but paused. What was her campus username again? DY3_1989 or 3DY_1989?
Finally, she made it just in time. As she took her seat, a colleague leaned over and whispered, “Everything okay, Dawn?”
“Oh yes, of course. I just missed the email about the room change,” she replied.
Her colleague looked puzzled. “But Dawn, I thought we agreed to change it last week because of the maintenance? You sent out the updated flyer.”
Another tile falls
Dawn had imagined the end of her professional life – more often now with retirement approaching. She thought it would be a graceful exit after decades of research. She might face a diagnosis with late-onset breast cancer like her mother at this age, but she will confront it with the same precision and drive she’d applied to everything else. Or she might go climb the Alps. Or she might just lie down for two weeks and do absolutely nothing.
Dementia was never part of that future.
It began subtly. Small moments. A cup of coffee left untouched. Typos in emails. Hesitations before recalling the name of the protein she’d studied for two decades. She thought it was stress. Or age. Or simply just not enough caffeine. Nothing serious and surely nothing she couldn’t resolve.
Then came the gaps. Experimental updates she had asked about but couldn’t recall. A library book she didn’t remember borrowing. A missed dinner with her daughter that she forgot had even been planned.
“I remember walking back to my office after the seminar,” she said to her doctor, “but not the seminar itself. It felt like remembering a dream—except I am not sure I actually had it.”
Her primary care doctor hesitated. “Fatigue,” he suggested. “You’re retiring soon – maybe it’s just nerves.” But the symptoms grew louder. Trouble focusing. Misplaced objects. Stumbling through tasks she used to perform effortlessly.
A diagnosis that sticks
A lumbar puncture confirmed the presence of biomarkers for Alzheimer’s disease. Her neurologist tried to reassure her: “It’s manageable. There are medications that have worked great for some patients.” She was put on donepezil at first, which brought mild clarity, but then as the dosage increased, the effect plateaued. And the eerie fog returned. Now, she has sticky notes in every room of her house. The most prominent reads: Replace rivastigmine patch at 8 a.m.
It won’t reverse the tide, but it gives her a little more time.
The diagnosis also came with something unexpected – but not unfamiliar: doubt. Not her own, but others: Colleagues began to slow their speech. Friends over-explained simple things. Her daughter gently suggested she stop driving.
Now, she carries a small notebook to record what she reads, what she thinks, and what she forgets. Not in hopes of remembering later, but to give shape to the fog. And finally, when a fellow professor explained to her, “A western blot is used to detect specific proteins in a sample,” Dawn wrote:
I am the first female professor with tenure in this department. I pushed through gender bias and countless microaggressions until no one questioned my qualification. Now, someone slaps the label of ‘Alzheimer’s’ and I see the same doubtful looks I saw in 2001. Maybe they forgot that I am a scientist. Or maybe they are the ones with memory loss.
The many faces of loss: self and autonomy
Memory, of course, was at the center of it all. But it wasn’t just about forgetting names and places. It was the slow erosion of identity of self, of confidence, of the daily things that made her who she was.
Dawn once mistook the dishwasher for the washing machine.
She forgot the name of her first graduate student—now a leading immunologist who had sent flowers on the day of her retirement.
She tried to stay up to date with the latest research, only to find the exact same article printed three times on her nightstand, each version heavily annotated with the same short notes.
She clings to routine now: Breakfast at 7. Rivastigmine patch at 8. Swim at 8:30. Two easy-level Sudoku puzzles in the afternoon.
She writes more and more into her notebook, trying to anchor herself to something tangible.
The word that could not be said
“Alzheimer’s” was the word Dawn avoided for a long time. It felt too heavy, like a ketchup-and-mustard stain on a white shirt – impossible to ignore and impossible to clean.
“Why couldn’t Alois Alzheimer have had a gentler last name?” she once joked. “What about Alois Baker? That sounds friendlier. Oh I should write that down.”
She saw it in people’s faces: discomfort, pity, softened expressions. Once, she overheard someone say, “It’s such a shame—she was so smart.” As if she had already died. As if her mind and her life no longer counted.
So she minimized it. “Just part of getting older”, she’d say, “a bit more forgetful.” Like many others in her position, she tried to hide her symptoms. She redirected conversations when the subject comes up, but not out of shame. She tried really hard to protect her dignity and preserve her autonomy.
But eventually, she got angry.
She was still herself. She was still here.
No more “How ARE you?” or “It’s okay if you don’t remember.” She began to speak about her experience – openly, honestly, without fanfare. She answered questions. She explained what was happening. And something shifted.
People opened up to her. About their own forgetfulness. Their aging parents. Their fears of growing older. Instead of turning away, they learned in to listen.
She was still teaching, in her own way.
Navigating independence

Dawn cannot imagine living in a care home.
She values independence not only as a lifestyle but also as a principle. The thought of being fussed over, corrected, or guided like a child feels unbearable.
And yet, she adapts.
A part-time caregiver visits three times a week. Friends walk with her on familiar trails. Her daughter installed a GPS tracker on her phone – just in case.
She continues, like so many living with dementia, to build a life within shifting boundaries. She reads. She writes. She cooks simple meals. She builds small rituals that keep her grounded.
On a walk with a friend, she said:
“Some days, I forget where I left the book I was reading. Or what I was reading. So I start again. I read the preface over and over. Each time, it’s almost like reading it for the first time. There’s something… kind about that. Maybe for everything I lose, I can always try to learn it again.”
Back to the beginning
Dementia doesn’t rudely erase a person all at once. It softens the edges, yes – but it also reveals what endures.
Dawn no longer teaches. She no longer drives. She doesn’t always remember the papers she published or the students she taught. But she still feels the pulse of who she is.
Some days are clearer than others. Some are quiet and uneventful. Still, she holds onto the rituals that tether her to herself: morning coffee, music in the afternoons, crosswords even when they don’t quite land.
She keeps a photo of herself in her first lab beside her bed. One night, she picked it up and smiled; not at the outdated centrifuge or the cluttered bench, but at the young woman in the photo, standing with her arms crossed, looking entirely at home.
I was someone who knew things, she assured herself. And I still am.
Footnote
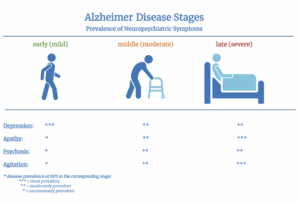
The depiction of Alzheimer’s disease and its effects in this story draw on a range of research and clinical studies that documents the progression, impact, and treatment of Alzheimer’s disease over time. The studies referenced below trace the clinical, psychological, and social dimensions of the illness in chronological orders:
- Zubenko, George S et al. “A collaborative study of the emergence and clinical features of the major depressive syndrome of Alzheimer’s disease.” The American journal of psychiatry vol. 160,5 (2003): 857-66.
- de Boer, Marike E et al. “Suffering from dementia – the patient’s perspective: a review of the literature.” International psychogeriatrics vol. 19,6 (2007): 1021-39.
- Burke, Anna D et al. “Diagnosing and Treating Depression in Patients with Alzheimer’s Disease.” Neurology and therapy vol. 8,2 (2019): 325-350.
- Atri, Alireza. “The Alzheimer’s Disease Clinical Spectrum: Diagnosis and Management.” The Medical clinics of North America vol. 103,2 (2019): 263-293.
- Wolfe, Sarah E et al. “The meaning of autonomy when living with dementia: A Q-method investigation.” Dementia (London, England) vol. 20,6 (2021): 1875-1890.
- Tahami Monfared, Amir Abbas et al. “A Systematic Review of Clinical Practice Guidelines for Alzheimer’s Disease and Strategies for Future Advancements.” Neurology and therapy vol. 12,4 (2023): 1257-1284.
- Fisher, Daniel W et al. “Distinguishing features of depression in dementia from primary psychiatric disease.” Discover mental health vol. 4,1 3. 4 Jan. 2024.
- Nandi, Arindam et al. “Cost of care for Alzheimer’s disease and related dementias in the United States: 2016 to 2060.” NPJ aging vol. 10,1 13. 8 Feb. 2024.
- Zhang, Jifa et al. “Recent advances in Alzheimer’s disease: Mechanisms, clinical trials and new drug development strategies.” Signal transduction and targeted therapy vol. 9,1 211. 23 Aug. 2024.
- Li, Jing et al. “Alzheimer’s disease with depression: clinical characteristics and potential mechanisms involving orexin and brain atrophy.” Translational psychiatry vol. 15,1 66. 24 Feb. 2025.
- Anselmo, Anna et al. “Beyond Diagnosis: Exploring Residual Autonomy in Dementia Through a Systematic Review.” Medicina (Kaunas, Lithuania) vol. 61,5 895. 14 May. 2025.
Peer Editor: Grace Stroman and Elizabeth Abrash