Blood is essential. It carries the oxygen you breathe throughout your body and to your lungs, keeping you alive and invigorated. However, our body can only produce so much blood in a day, and when we undergo serious blood loss through car accidents, genetic disorders, or surgeries, we need to replenish our body’s blood supply. People around the world donate their blood to those who are in desperate need and each year, 4.5 million lives are saved thanks to blood donations.
The transfer of one person’s blood to another person’s body is called transfusion, and in the United States alone, someone needs a transfusion every two seconds1. Currently, blood transfusions are limited by the type of blood one has – and therefore needs. Blood has four major types: ‘A’, ‘B’, ‘AB’, and ‘O’, and each of these major types has two subtypes, positive or negative. This means there are a total of eight blood types: A+, A-, B+, B-, AB+, AB-, O+, O-. These types are determined by different molecules called antigens (you can think of them as tags or signs) on the outside of the blood cell (see image below, different blood types have different molecular patterns or “tags”).
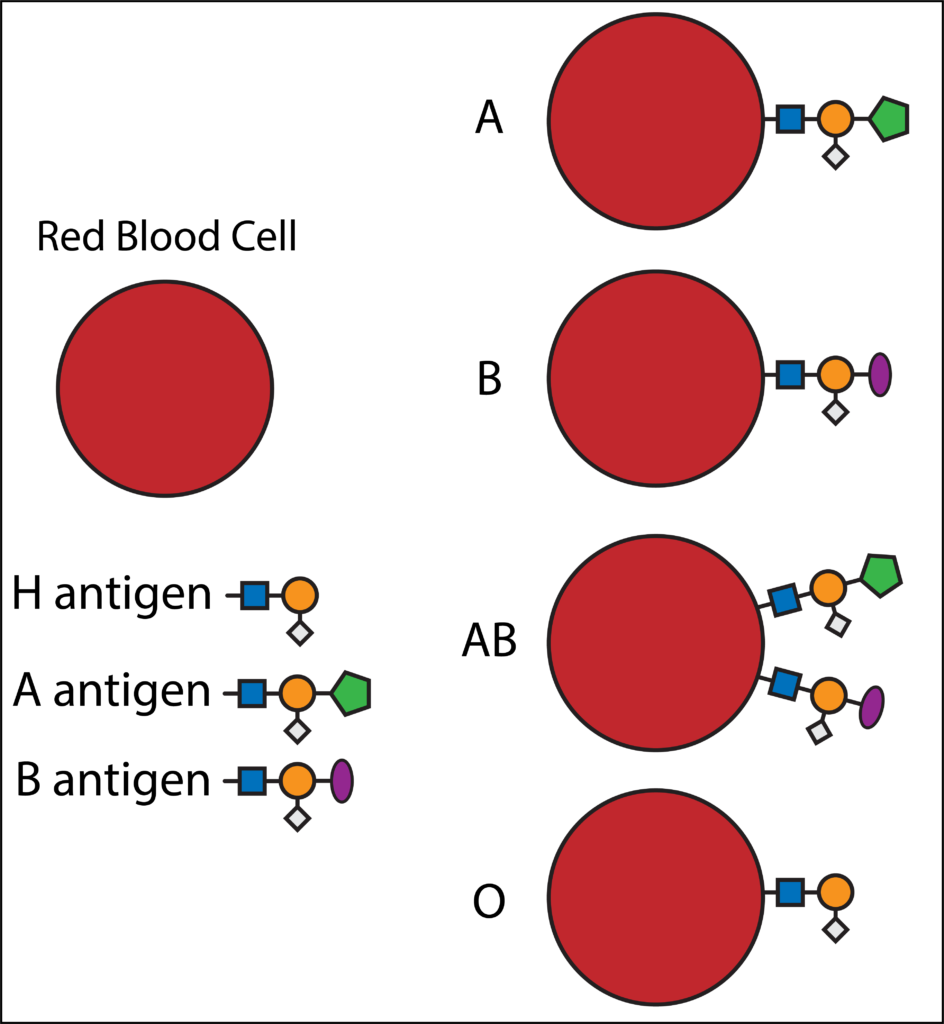
Blood transfusions are limited by these specific antigens (tags) because the antigens are recognized by a person’s immune system or, the body’s defense system. If you have blood type “B”, and now have blood type “A” in your body, due to a transfusion, your immune system will recognize that “A” is not part of your body, and will trigger an immune response which attacks and destroys the blood that has been transfused.
A group from the University of British Columbia in Canada identified a bacterium in the human stomach that can convert blood type ‘A’ to the universal donor type, ‘O’2. By screening thousands of microbes in our stomachs, the scientists identified a particular obligate anaerobe (can only survive when oxygen is not present), Flavonifractor plautii. Inside F. plautii, two enzymes were found to work together to change the molecules on the surface of red blood cells of blood type ‘A’ to molecules of blood type ‘O’.
But how can blood types be changed from one blood type to another?
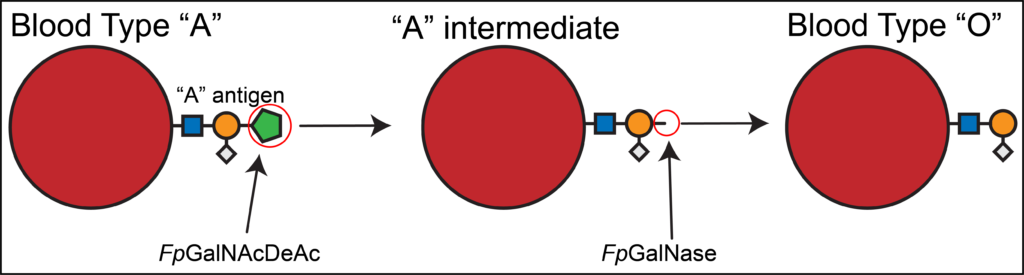
Below is a diagram of blood type ‘A’ and blood type ‘O’. They have some “tags” in common (the blue squares, orange circles, and grey diamonds), and some that differ (green pentagon). The enzymes in F. plautii are able to cut off the extra molecular tag of blood type ‘A’, which then leaves blood type ‘O’! First, the enzyme FpGalNAcDeAc changes the ‘A’ blood type molecules to a slightly different molecule, which can then be recognized and cut by the second enzyme, FpGalNase, leaving blood type ‘O’. Not only can these enzymes change blood type ‘A’ to ‘O’, but they can do it fairly efficiently, which could greatly increase the blood supply for transfusions.
The group from British Columbia are not the first to try changing blood type3. A previous study converted blood type ‘B’ to blood type ‘O’, albeit very inefficiently. So inefficiently, in fact, that the conversion would never have practical use4.
Since the enzymes from F. plautii are bacterial, and only small amounts of the enzymes are needed for conversion of blood type ‘A’ to blood type ‘O’, it could be possible to mass produce the enzymes to be able to transform large quantities of blood for transfusions, increasing blood supply for medical procedures and saving more lives.
Sources:
- https://www.redcrossblood.org/donate-blood/blood-types.html
- Rahfeld, P., Sim, L., Moon, H., Constantinescu, I., Morgan-Lang, C., Hallam, S. J., Kizhakkedathu, J. N., and Withers, S. G. (2019) An enzymatic pathway in the human gut microbiome that converts A to universal O type blood. Nat. Microbiol. 10.1038/s41564-019-0469-7
- Goldstein, J., Siviglia, G., Hurst, R., Lenny, L. & Reich, L. Group-B erythrocytes enzymatically converted to Group-O survive normally in A, B, and O individuals. Science 215, 168–170 (1982).
- Kruskall, M. S. et al. Transfusion to blood group A and O patients of group B RBCs that have been enzymatically converted to group O. Transfusion 40, 1290–1298 (2000).
Peer edited by Abigail Agoglia
Interesting. As long as the process does not otherwise adversely affect the red cell membrane, the next step would be to enzymatically remove the RH antigens. Then you’d really have something!
I had RH incompatibility as a child in 1968 and had several blood exchanges. My blood type was A and it changed to O after the exchanges.