Around the world, people’s lives have been dramatically impacted by the novel coronavirus SARS-CoV-2, which causes the disease known as COVID-19. There are a lot of unknowns when it comes to SARS-CoV-2, including whether using electronic cigarettes, or e-cigarettes, can increase someone’s risk for becoming sick with this virus. While no studies about how e-cigarette use affects COVID-19 have been published, experts from the National Institute on Drug Abuse and American Lung Association have warned that using e-cigarettes could increase risk for COVID-19 by generalizing from what we already know about the way vaping impacts the respiratory immune system.
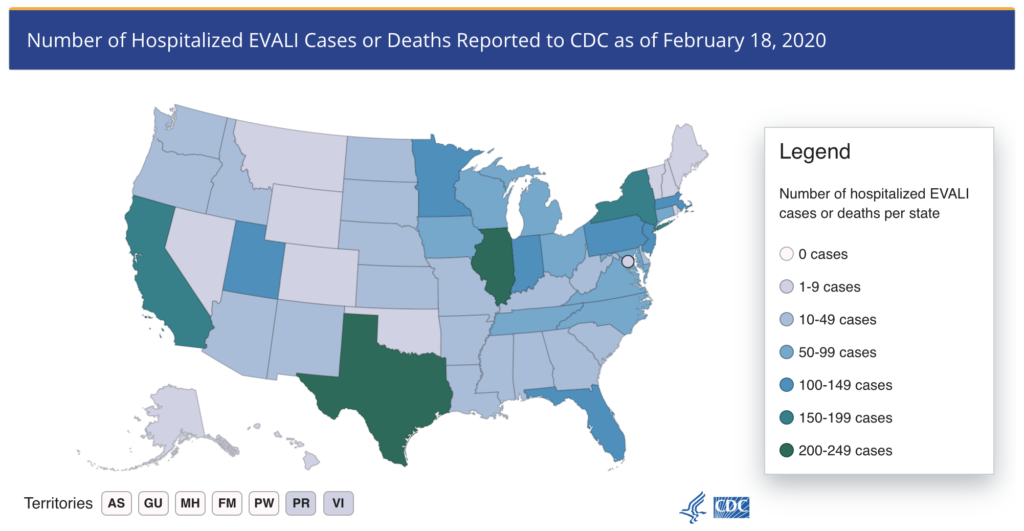
Map of lung injury cases reported to the CDC. Source: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html
A few months before the COVID-19 pandemic began, e-cigarettes made the national news because there was an outbreak of over 2500 cases of E-cigarette or Vaping product use Associated Lung Injury (EVALI) reported in 50 states (Figure 1). 68 deaths have been attributed to EVALI, and physicians and scientists are still trying to understand the cause of these recent acute illnesses. Even though data collected by the CDC links vitamin E acetate contamination of THC (tetrahydrocannabinol – the main active ingredient in marijuana) vaping products to EVALI, we still don’t know the exact mechanism linking vitamin E acetate to EVALI.
The potential health effects of long-term e-cigarette use are still largely unknown. A timely paper published in September 2019 in the Journal of Clinical Investigation used mice to study the effects of long-term e-cigarette exposure on the lungs. They found that mice exposed to e-cigarettes had decreased ability to fight a flu infection because the immune cells in their lungs were not functioning correctly.
In the study, mice were exposed five days a week to unflavored e-cigarette aerosol from a vape pen, with or without nicotine (an addictive substance found in tobacco products), for four months. (Figure 2) For comparison, another group of mice was exposed to fresh room air, and a fourth group of mice was exposed to cigarette smoke. The researchers first looked to see if these exposures resulted in inflammation in the lungs, and they found that only the mice exposed to cigarette smoke had lung inflammation. However, when the researchers looked more closely at specific cells in the lungs, they saw that there was a lot of lipid, or fat, in the cells of the mice exposed to e-cigarettes but not mice exposed to fresh air or cigarette smoke.
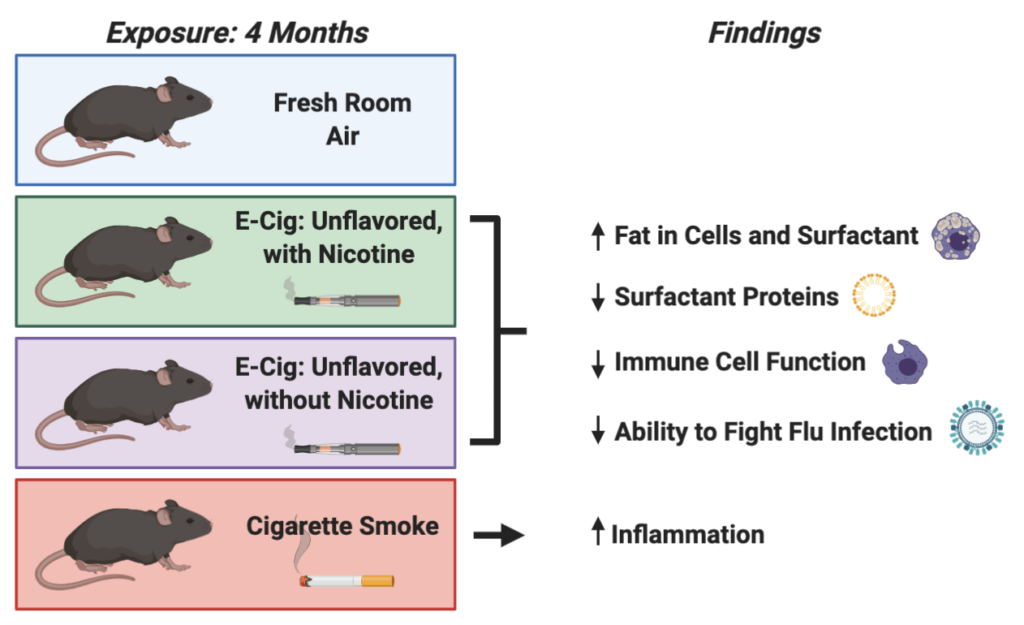
Why is fat in the lungs important? The lungs are lined with fluid called surfactant that helps maintain lung structure and protects the lungs from infection. Surfactant is made up of lipids and proteins, and both immune cells and lung cells help determine the amount and composition of surfactant. Changes in the composition of surfactant can result in decreased lung function and increased susceptibility to infection.
Because e-cigarette exposure affected components in the lung associated with immune defense, the researchers wanted to test how e-cigarette-exposed mice would respond to flu infection. In comparison with unexposed mice, the mice exposed to e-cigarettes with or without nicotine were less able to clear the virus and survive the infection. Their lungs were much more inflamed, and they had a lot more tissue damage as a result of flu infection. This study is important because it adds to our understanding of the potential health consequences of chronic e-cigarette use and presents new ideas for scientists to follow up on in future e-cigarette research
The findings of this study suggest that e-cigarettes can disrupt lipid balance in the lungs resulting in impaired response to flu infection, which has implications for the lung’s ability to fight viral infections in general, including infections with SARS-CoV-2. These findings are in agreement with previous research showing decreased immune function as a result of e-cigarette exposure, and they provide promising avenues for researchers to pursue in follow-up studies.
However, it is important to keep in mind that this study was performed in mice and that these effects will need to be confirmed in human e-cigarette users. In addition, men are more likely to use e-cigarettes and more men have been sick in the recent outbreak, but this study only used female mice. Other components of this study that will need to be researched further include determining the role of flavoring chemicals in altering these effects and whether other types of e-cigarette devices that are currently popular, such as box mods and JUULs, similarly change the function of immune cells in the lungs.
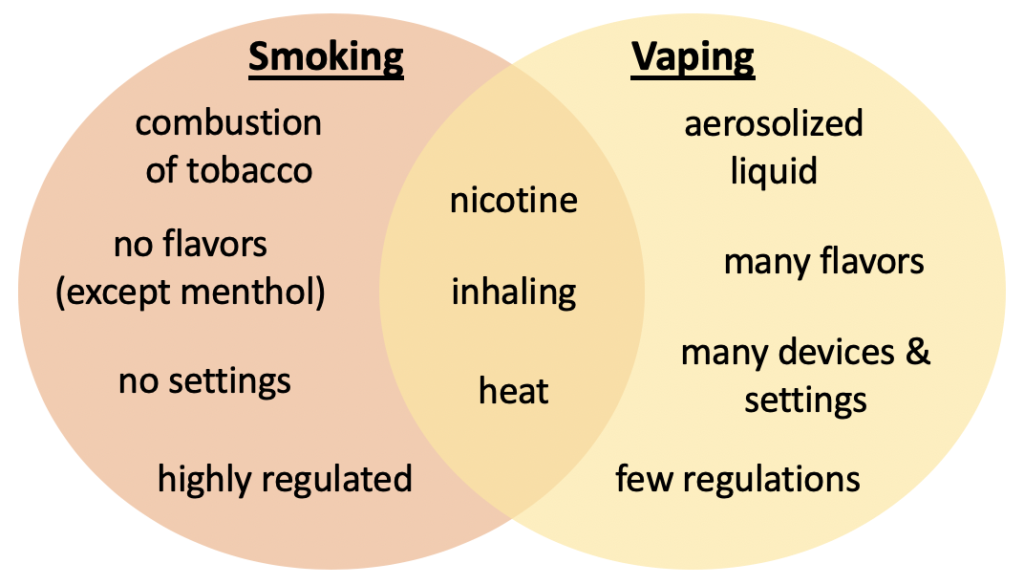
It is also important to note that the frequent comparison of the cancer risk between e-cigarettes and cigarettes does not represent a full range of possible health consequences. The study discussed in this article highlights how the effects of e-cigarette use are likely unique from, rather than on the continuum of, health effects that occur as a result of smoking. This makes sense, as e-cigarettes create a chemical exposure that is very different from cigarette smoke (Figure 3). And, despite the need for more research on e-cigarettes, it is becoming clear, due to the recent cases of EVALI, that using e-cigarettes has health consequences beyond those of nicotine alone. It may take time for these consequences to become fully realized, but it is critical for the public to understand that there are unknown risks associated with e-cigarette use, so that they can make informed decisions regarding these devices.
Peer edited by Rachel Ernstoff